MSOME: the semen analysis of the future
The semen analysis is the basic diagnostic test for male fertility. It involves analysing the different semen parameters, such as the concentration of spermatozoa, their motility, vitality and morphology etc. However, various studies have shown that these parameters can vary significantly, even for the same individual. That is to say that the same person can have very different results depending on when the semen analysis is carried out. Evidently, this makes diagnosis and selecting the most appropriate assisted reproduction technique more difficult, thus reducing the probability of success.
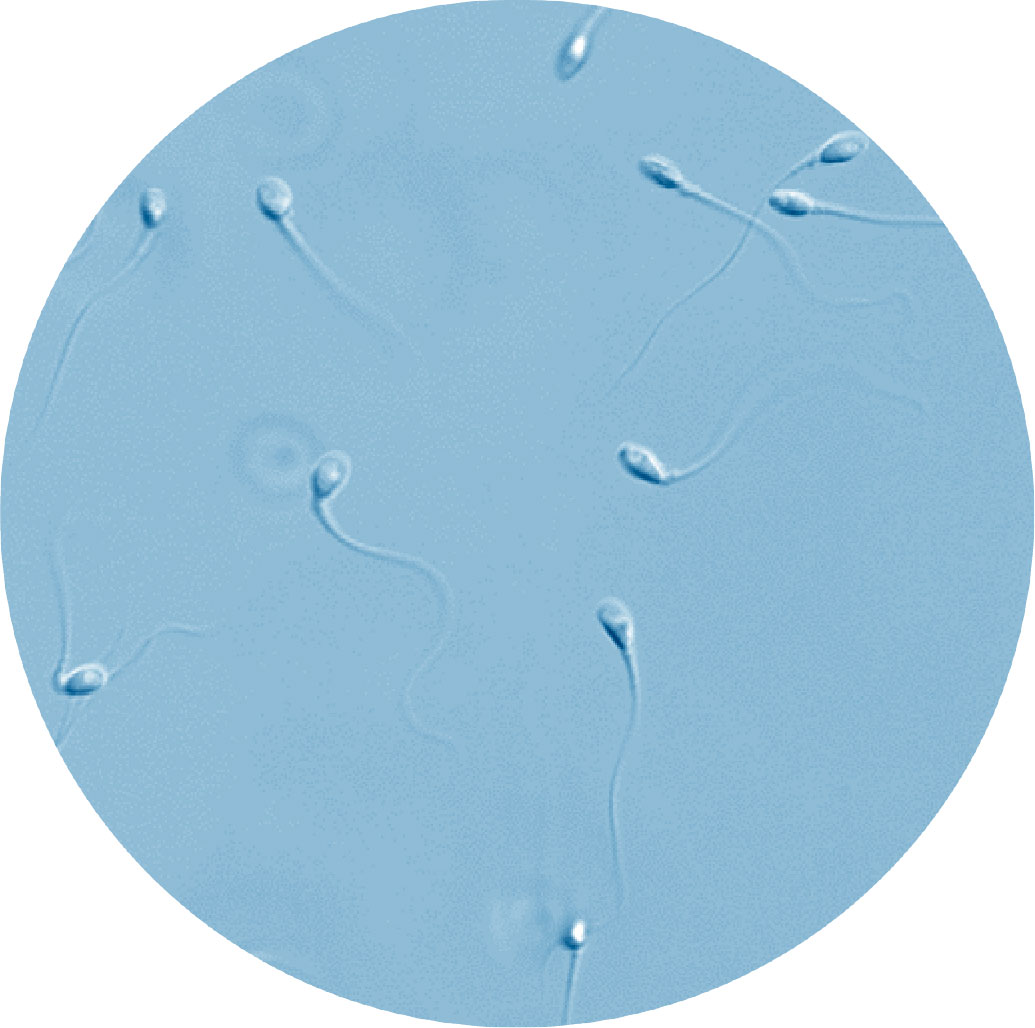
conventional semen analysis
400X
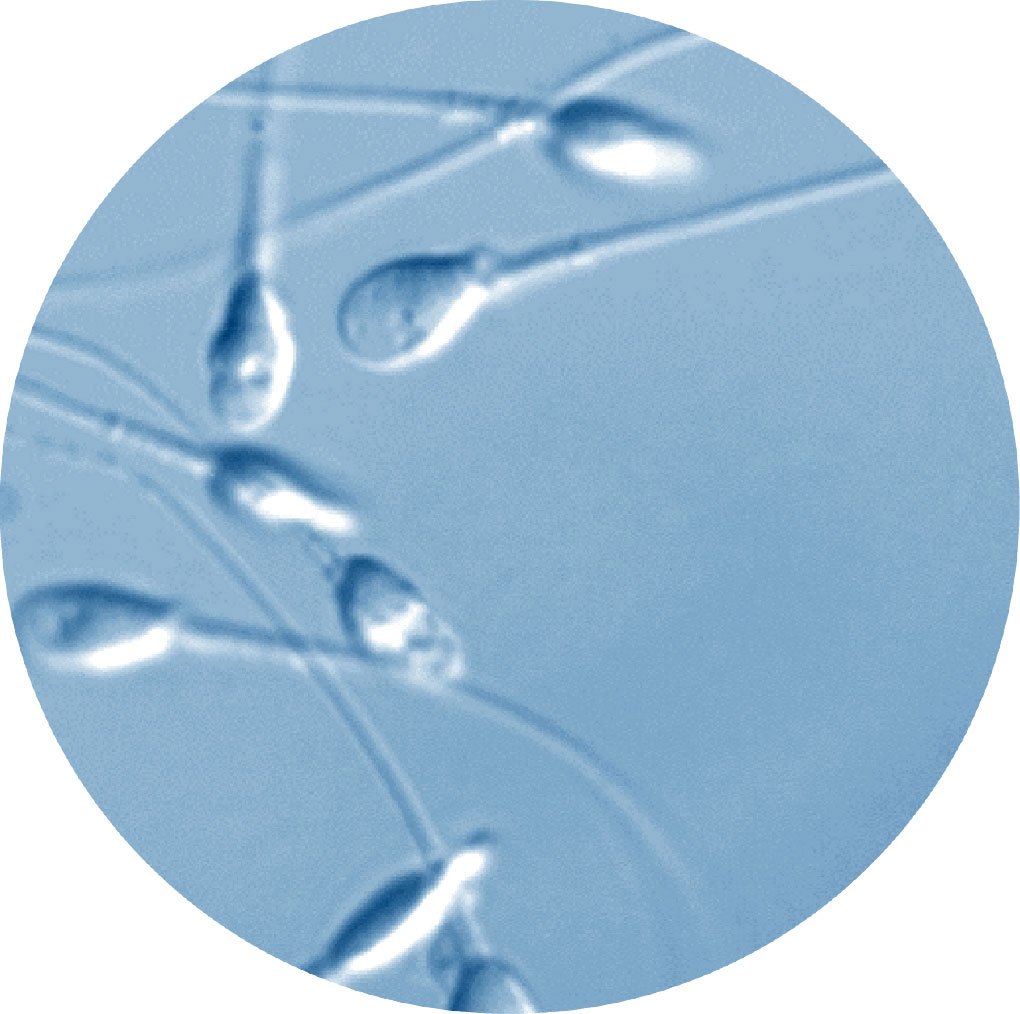
MSOME semen analysis
10.000X
What is MSOME?
MSOME or Motile Sperm Organelle Morphology Examination is a new test that allows sperm morphology to be evaluated in real time to a very high degree of accuracy. While conventional sperm analysis is carried out under a magnification of between 200 and 400, this new MSOME technology, analyses spermatozoa under a magnification of 10,000. Recent studies have shown that the results obtained using MSOME remain unaltered for months, and, thus, provide vital information for assessing spermatozoa quality.
What is MSOME used for?
While traditional methods of analysing male fertility provide extremely superficial information, the MSOME test is able to identify spermatozoa with an altered nucleus, that is to say, with potentially damaged DNA or genetic material. This means that these can be separated from those with a good morphology that are capable of creating better quality embryos (with a higher chance of pregnancy and a lower risk of miscarriage).
What are the advantages of MSOME?
The main advantage is that in addition to providing information regarding sperm quality, MSOME allows us to guide the patient towards using either a “conventional” assisted reproduction technique or towards IMSI (where the oocytes are microinjected with spermatozoa that have been previously selected by MSOME).
For whom is MSOME indicated?
Everyone can have a MSOME test, however, it is particularly indicated for those men with an altered semen analysis or those who have had previous unsuccessful assisted reproduction cycles.




 Español
Español Français
Français Català
Català Italiano
Italiano Русский
Русский